What is strabismus and how common is it?
Strabismus is any misalignment of the eyes. It is estimated that 4% of the U.S. population has strabismus.
Are there different types of strabismus and if so, how are they named?
There are many different types of strabismus. Strabismus is most commonly described by the direction of the eye misalignment; common types of strabismus are esotropia, exotropia, hypotropia, and hypertropia.
Strabismus can also be described by its cause. The 3 cranial nerves (III, IV, VI) responsible for eye movement can be weak or palsied and cause strabismus. Some examples of paralytic strabismus include third nerve palsy and superior oblique palsy.
Special patterns of strabismus can have unique names such as Brown syndrome, and Duane syndrome.
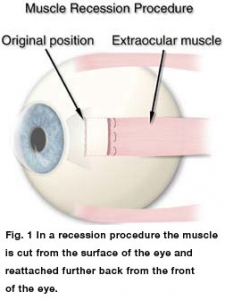
Figure 1
What are the types of horizontal strabismus?
Esotropia is inward turning of the eyes (aka “crossed eyes”). Types of esotropia include infantile esotropia, accommodative esotropia, and sixth nerve palsy. Exotropia is the term used to describe outward turning of the eyes (aka “wall-eyed”)
[See figures 1 and 2].
What are the types of vertical strabismus?
The terms hypertropia and hypotropia are used to describe vertical misalignment. Hypertropia is an abnormal eye higher than the normal eye. Hypotropia is when the abnormal eye is lower than the normal eye. The terms can generally be interchanged.
What causes strabismus?
Most strabismus is the result of an abnormality of the poorly understood neuromuscular (including brain) control of eye movement. Less commonly, a problem with the actual eye muscle causes strabismus.
How is strabismus related to poor vision?
Eye misalignment can cause amblyopia in children. When the eyes are oriented in different directions, the brain receives 2 different visual images. The brain may ignore the image from the misaligned eye to avoid double vision, resulting in poor vision development of that eye. Also, an eye that sees poorly tends to be misaligned.
Who develops strabismus as a child?
Strabismus often occurs in children who are otherwise completely normal. However, disorders that affect the brain such as cerebral palsy, Down syndrome, hydrocephalus and brain tumor are more likely to develop strabismus.
What adult disorders cause strabismus?
Stroke is the leading cause of strabismus in adults. Trauma, neurological problems, and Graves disease (thyroid eye disorders) are other common causes of strabismus.
How does trauma cause strabismus?
Trauma can cause strabismus by 1) brain damage that impairs control of eye movement, 2) damage of the nerves that control eye movement and/or 3) damage of the eye muscles either directly or secondarily from trauma to the eye socket.
How is strabismus treated?
The goal of strabismus treatment is to improve eye alignment which allows for better work together (binocular vision). Treatment may involve eye glasses, eye exercises, prism, and/ or eye muscle surgery. Problems associated with strabismus (including amblyopia, ptosis, and cataract) are usually treated prior to eye muscle surgery.
What is strabismus surgery?
Strabismus surgery loosens or tightens eye muscles, which changes the alignment of the eyes relative to each other.
What kind of anesthesia is used for strabismus surgery?
The type of anesthesia depends on age/health and patient preference. Most children undergo general anesthesia. Adults typically have general anesthesia, conscious sedation or local anesthesia. The procedure is usually performed as an outpatient (come in and go home the same day).
How does the surgeon approach the eye muscles?
The eye muscles attach to the sclera (wall of the eye). The muscles are covered by a thin layer of transparent tissue called the conjunctiva. The eyelids are held open by a small instrument called a lid speculum. The surgeon incises the conjunctiva to access the eye muscle(s), and uses a delicate hook to isolate the muscle. No skin incisions are made. The eyeball is NOT removed from the eye socket during strabismus surgery.
What is a recession?
A recession weakens function by altering the attachment site on the eyeball. A suture is placed through the muscle at the attachment site to the eye. The muscle is cut from the surface of the eye and reattached further back from the front of the eye [See figure 1].
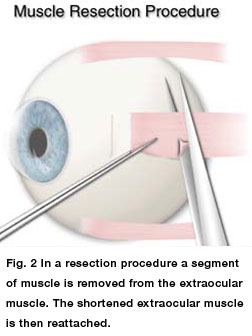
Figure 2
What is a resection?
A resection strengthens function by reattaching a muscle to the eyeball at the original insertion site after a portion is removed. A suture is placed through the muscle at the intended new attachment site. The segment of muscle between the suture and the eyeball is removed and the shortened muscle is reattached to the eye [See figures 2 and 3].
What is an adjustable suture?
Strabismus surgery involves sewing the eye muscle to the wall of the eye after altering the insertion position and/or the length of the muscle. Standard strabismus surgery (no adjustable suture) utilizes a permanent knot. Adjustable suture technique utilizes a bow-knot or slip-knot (temporary knot) in an accessible position. After surgery the eye alignment can be altered by adjusting the temporary knot. The adjustment is typically done while awake and the operated eye numbed.
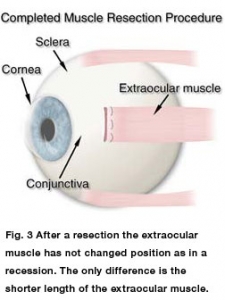
Figure 3
Are the eyes red after strabismus surgery?
It is normal for the white part of the eyes to be red after surgery. It may take several weeks/months for the redness to disappear. The eyes are usually scratchy and are sore upon movement. The soreness usually improves after a few days.
Are patches or medicine used after surgery?
A patch is usually placed only if an adjustable suture is used. Some surgeons prefer an antibiotic or combination antibiotic/steroid drop or ointment after surgery.